Guest Blog By: Anneka Hofschneider, MA, BCBA, CBIS
 I first got my taste for neurorehabilitation as a student intern in the summer of 2010. By attending California’s Association of Behavior Analysis and Association for Behavior Analysis International’s Annual Conferences, I was introduced to my current place of employment and the opportunities for a Board Certified Behavior Analyst (BCBA) in Brain Injury. I have been consistently working in the field since 2013. BCBAs working in brain injury account for 0.09%, according to the certificant data on the BACB’s webpage. Though we are few, we fiercely take on this endeavor. I take pride in this statistic and find many sources of reinforcement in my current career path. There is a great reward to working with this challenging demographic and I am honored to share some examples of how my colleagues and I have incorporated behavior analysis – specifically, verbal behavior – into our work.
I first got my taste for neurorehabilitation as a student intern in the summer of 2010. By attending California’s Association of Behavior Analysis and Association for Behavior Analysis International’s Annual Conferences, I was introduced to my current place of employment and the opportunities for a Board Certified Behavior Analyst (BCBA) in Brain Injury. I have been consistently working in the field since 2013. BCBAs working in brain injury account for 0.09%, according to the certificant data on the BACB’s webpage. Though we are few, we fiercely take on this endeavor. I take pride in this statistic and find many sources of reinforcement in my current career path. There is a great reward to working with this challenging demographic and I am honored to share some examples of how my colleagues and I have incorporated behavior analysis – specifically, verbal behavior – into our work.
Introduction to Brain Injury
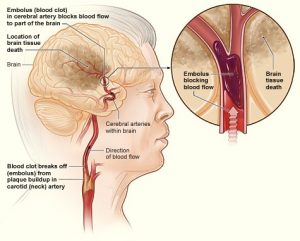
First, a quick overview on brain injury. Brain injuries may generally be classified as traumatic or non-traumatic. Traumatic brain injuries (TBI) are more common and are caused by an external force such as falls, motor vehicle accidents, gunshot wounds, assaults, and military actions to name a few (Center for Disease Control (CDC), 2019). According to the CDC, in 2014, nearly 2.8 million Americans were treated emergently because of a TBI, with an estimated 155 deaths per day. Non-traumatic injuries are caused by internal injuries such as stroke, infection, tumors, and loss of oxygen. Treatment for brain injuries can occur at the acute, post-acute, and long-term levels. Treatment may involve a multidisciplinary team consisting of neurologists, case managers, licensed clinicians (e.g., Physical, Speech, Occupational Therapists), counselors, and paraprofessionals. BCBAs can be an instrumental part of the team addressing skill deficits, problem behavior reduction, as well as staff and family training. Collaboration is key and has contributed positively to the many cases I have had the privilege to work on.
A common proverb in neurorehabilitation is “you see one brain injury, you’ve seen one brain injury”. Deficits, severity of injury, symptoms, and the course progression differ from person to person. The following are some basic illustrations of verbal behavior programming in brain injury rehabilitation.
Functional Communication Training in Brain Injury Rehabilitation
Functional communication within brain injury is of particular importance when working with escape-maintained behaviors. Neurorehabilitation is not without its demands and often, problematic behaviors (e.g., hitting, cursing, yelling) may serve to slow down or stop such demands. Verbal aggression has been identified in 34% of patients three months post-injury and up to 38% 12 months post-injury (Roy, Vaishnavi, Han, & Rao, 2017). Given the high shock value and low response effort, verbal aggression (i.e., cursing, yelling) is a common behavioral excess to address the following injury. Results from functional behavior assessments typically yield these behaviors to be escape-maintained. Our job is to teach better and appropriate ways of escaping as well as emphasizing the importance of function: that behavior is lawful and these individuals are not trying to be jerks, mean, or any other “personality trait” that fits the bill.
Now bring to the scene a diagnosis of aphasia: the acquired inability to comprehend or produce language. Behaviorally speaking, either speaker and/or listener behaviors may be affected. There are different types of aphasias, however, for the purpose of this entry, we will look at nonfluent aphasia. After suffering a thrombotic stroke (i.e., blood clot), a patient diagnosed with nonfluent aphasia with profound apraxia of speech (think of a disruption between brain signals to the mouth, tongue, lips impacting movement), presented with a minimized word repertoire of one to three words. For confidentiality, let’s say those three words were: heart, you, me. What later turned out to be the patient’s attempt at communicating a lost electronic device, the words “heart” and “you” were repeated over with variations in tone and prosody: “hearrrt”, “yooouu”, “you”, and so on. This presented an opportunity to evaluate the function of voice intonation with respect to their requests (i.e., mands) and labeling items (i.e., tacts). With aphasia, a person may be able to request “water”, but when presented with a cup of water have difficulties labeling “water”. Similarly, they may have a harder time repeating that the day is “Monday” as opposed to saying “Monday” when repeating the days of the week sequentially (i.e., Sunday, Monday, Tuesday…). A person with aphasia may also be more likely to follow a directive when written compared to if it was spoken, or vice versa. These interesting phenomena can be accounted for from a behavior analytic perspective. If the reader would like a more detailed explanation of this, Baker, LeBlanc, and Raetz (2008) provide a behavioral interpretation of aphasia addressing the aforementioned illustrations.
Take another patient who suffered a severe TBI secondary to a complex skull base fracture, falling 30 feet from a roof. Following this injury, the patient was limited to a wheelchair for mobility and highly dependent on others for all activities of daily living. Additionally, speaker behavior was limited to: gesturing to communicate “yes” with two fingers and “no” with one finger, a thumbs up, or thumbs down. After an intensive bowel and bladder management program targeting continence, detection/awareness, and initiation, we needed a proxy to serve for initiation. We introduced a standard game buzzer with the instructions “push the buzzer if you need to use the restroom”. After several independent occurrences of buzzer-pushing for restroom use, we observed this behavior to generalize to requesting (i.e., mand) for attention from staff such as when a towel dropped to the floor requiring staff to pick it up for the patient. Needless to say, buzzers and other forms of auditory alerts (i.e., call bells) continue to be used to help with initiation and communication.
Differential Reinforcement Strategies with TBI Patients
 We may also serve as the ever-important audience for patients rehearsing strategies. A patient diagnosed with post-concussion syndrome following a motor vehicle accident presented with a functional motor speech disorder characterized by stuttering. Our responses as audience members provided differential reinforcement for strategies including speaking slower, enunciating, and self-correction (e.g., responding when these strategies were used and asking for clarification if not). Another critical role as an audience member is in the extinction of perseverative speech, as in the case of a patient diagnosed with a TBI following a motorcycle vs. car injury. This individual’s pre-injury employment required active and frequent questioning with most individuals encountered. This repertoire increased and occurred at high frequencies interrupting conversations, escalating behaviors when unanswered, and encouraging socially inappropriate behaviors (e.g., “are you married?”, “will you go out with me?”). Thus, a program outlining for staff to respond and engage when the patient asked or made context-appropriate questions/ statements were implemented to address these behaviors.
We may also serve as the ever-important audience for patients rehearsing strategies. A patient diagnosed with post-concussion syndrome following a motor vehicle accident presented with a functional motor speech disorder characterized by stuttering. Our responses as audience members provided differential reinforcement for strategies including speaking slower, enunciating, and self-correction (e.g., responding when these strategies were used and asking for clarification if not). Another critical role as an audience member is in the extinction of perseverative speech, as in the case of a patient diagnosed with a TBI following a motorcycle vs. car injury. This individual’s pre-injury employment required active and frequent questioning with most individuals encountered. This repertoire increased and occurred at high frequencies interrupting conversations, escalating behaviors when unanswered, and encouraging socially inappropriate behaviors (e.g., “are you married?”, “will you go out with me?”). Thus, a program outlining for staff to respond and engage when the patient asked or made context-appropriate questions/ statements were implemented to address these behaviors.
The collaboration of BCBAs and SLPs with Verbal Behavior Programming
Collaboration with Speech Language Pathologists (SLPs) allows us exposure into cognitive rehabilitation (our SLPs address related areas including cognition, memory, and attention to name a few). Complexity increases when we consider our clinic-specific curriculum: the Cognition Module. The Cognition Module, implemented by our Cognitive Rehabilitation department, “begins with the basic concept of identifying perceptual features or objects (shape, color size). Therapists build on this foundation in exercises for patients who experience language impairments in memory, attention, problem solving, and categorization” (Centre for Neuro Skills, 2021). Our involvement with the Cognition Module may be direct (i.e., receiving training to run trials of the Cognition Module when working with patients) and indirect (i.e., behavior programming for refusals or avoidance as difficulty increases with improved performance (e.g., progressing up the levels of the Cognition Module). A fellow BCBA is also a licensed SLP who treats patients more directly within Cognitive Rehabilitation, on occasion, while incorporating behavioral principles. The average time to complete the multi-level curriculum is three months and can be modified if needed. Completing the Cognition Module is no easy feat and rightfully so, celebrated. Our time observing, discussing, and collaborating with our SLPs yield invaluable lessons and information: from the anatomical and mechanical workings of communication and swallowing disorders to patient-specific strategies and techniques. This provides us opportunities to expand our degree of analysis and treatment.
Working with patients with brain injuries is both highly demanding and rewarding. The demand is to deliver quality and uncompromised behavior analytic service, adhering to ethical principles and codes, working with a multi-disciplinary team, and often hitting the ground running in a race against limited insurance authorization periods. The rewards are tenfold these demands: disseminating behavior analytic principles to patients, families, stakeholders, and professionals; exploring creative ways of addressing problem behaviors and teaching skills; and, contributing to opportunities for a patient’s verbal behavior development to promote interactions with their environment, access reinforcement, and ultimately restore a normal rhythm of living – one which has been interrupted by an injury. That is the reward.
(Author’s Note: Thank you to all my colleagues who contributed to this entry and for their tiring and selfless work.)
Images are from www.neuroskills.com and www.clinicalcorrelations.org
 Anneka Hofschneider is a practicing Board Certified Behavior Analyst at the Centre for Neuro Skills in Bakersfield, CA. She has been working in neurorehabilitation since 2013. She is a Certified Brain Injury Specialist (CBIS) and an instructor for training curricula including: Everyday BehaviorToolsTM, ProACTR crisis management, and the ACBIS Fundamentals certificate. Her interests include therapeutic compliance and caregiver training.
Anneka Hofschneider is a practicing Board Certified Behavior Analyst at the Centre for Neuro Skills in Bakersfield, CA. She has been working in neurorehabilitation since 2013. She is a Certified Brain Injury Specialist (CBIS) and an instructor for training curricula including: Everyday BehaviorToolsTM, ProACTR crisis management, and the ACBIS Fundamentals certificate. Her interests include therapeutic compliance and caregiver training.
