For this month’s blog, I asked my friend and colleague, Dr. Ryan Olson, to tell our audience about the collaborative work he is doing on sleep, particularly as it relates to the workplace. Ryan asked his collaborator, Dr. Andrew McHill, to join (see their bios at the end). I am so pleased they have contributed this fascinating glimpse into their work, and I hope it inspires others to explore this area of research.
Sleep, Circadian Biology, and Health: Action in the Behavioral Interactions!
Andrew McHill, PhD
Ryan Olson, PhD
Oregon Institute of Occupational Health Sciences
Oregon Health & Science University
Portland, OR
We would like to encourage more behavioral psychologists to learn about and study sleep and circadian physiology, their interactions with daily behaviors, and the health and safety outcomes of such interactions. To do this we will share a few highlights from our own, and others’ research. In our view, collaborations between sleep and circadian physiologists and behavioral psychologists present rich opportunities for individuals to learn, make scientific discoveries, and develop effective interventions. However, we must confess to being somewhat biased, as we represent just such a collaborative team (Andrew is a physiologist, Ryan is a behavioral psychologist)!
Sleep deficiency, which can include insufficient sleep quantity or quality, is associated with poor health, chronic disease, and even early death (McHill & Wright, 2017). Sleep deficiency also causes fatigue and performance failures that can lead to serious injuries – at home or on the job. In fact, sleep deficiency, and the organizational systems that cause it, has been implicated as a major contributing factor in some of the worst industrial and environmental disasters (e.g., Exxon Valdez oil spill). Sleep deficiency, and its consequences, is estimated to account for an approximate $411 billion economic loss each year in the US alone (Hafner, Stepanek, Taylor, Troxel, & Van Stolk, 2017).
Why does sleep deficiency create these problems, and what can we do to improve sleep and prevent such bad things from happening? Sleep impacts on our health and safety are driven by genetic, physiological, and behavioral factors. In this blog, we focus on the latter two factors. It is an exciting area of research – there is much that is known, but also much to be discovered. There are also tremendous opportunities for sleep-informed interventions to improve human health and well-being.
Some of the health implications of sleep deficiency are illustrated by obesity and its associated health conditions. Sleep deficiency is quite strongly associated with obesity and chronic diseases like diabetes. It is thought that causal mechanisms may include how sleep insufficiency impacts our metabolism, food cravings, timing of calorie intake relative to the biological clock, and motivation to engage in other preventive health behaviors (e.g., exercise). Safety implications of sleep deficiency can be illustrated with a study of physicians. When physicians work extended (>24 hour) shifts they make more medical errors when compared to when they work shifts of shorter durations (Barger et al., 2006; Landrigan et al., 2004). And, it’s not just patients who are put at-risk: after an extended work shift physicians are at significant increased risk of being involved in a motor vehicle crash during their commute home (Barger et al., 2005).
In our own research, we have evaluated biological and behavioral mechanisms for relationships between sleep deficiency and health and safety outcomes. We have also evaluated interventions to improve sleep. Below we describe some of our own, and others’ studies on mechanisms and interventions.
Systemic, Physiological, and Behavioral Mechanisms
Organizational systems and working conditions can have strong impacts on sleep opportunities and sleep quality. Commercial truck drivers are exposed to a particular mix of working conditions that put them at-risk for sleep deficiency, weight gain, and poor health (Apostolopoulos, Sonmez, Shattell, & Belzer, 2010). Such conditions include long sedentary work hours, variable shift timing and night driving, limited opportunities and safe settings for physical activity, and “food swamp” conditions at truck stops. Among commercial truck drivers (n=452) we investigated patterns in self-reported health behaviors and their consequences. We used hierarchical cluster analyses to identify groups of drivers who had similar patterns in their self-reported eating, exercise, and sleep habits (Olson et al., 2016). Our goal was then to examine whether there were cluster differences in body mass index, chronic diseases, work stress, and work injuries and illnesses. The method identified five unique behavioral clusters of drivers. Two clusters, which we will refer to as Clusters A and B, provided a particularly interesting contrast. They were highly similar in the proportions of each cluster meeting behavioral health criteria for avoiding sugary drinks on most days each week (A=1.00, B=1.00), eating five fruits and vegetables a day (A=0.10, B=0.08), and 30 minutes of moderate physical activity on five days each week (A=0.15, B=0.11). Interestingly, both clusters had elevated levels of diabetes diagnosis, which may explain their avoidance of sugary drinks. However, Cluster A had the best sleep quality in the study, while Cluster B had the worst sleep quality in the study. How did Clusters A and B compare on other outcomes? Cluster B had significantly elevated work stress and lost work time due to injuries and illness. For Cluster A, their sleep sufficiency seemed to be protective – this cluster had some of the lowest levels of work stress and lost work time injuries and illnesses in the study.
In several separate studies, we have sought to identify how sleep timing, duration, and a person’s internal biological clock (i.e., the circadian clock) impacts energy metabolism and body composition. Other laboratories have shown that during controlled in-laboratory studies when sleep is experimentally shortened, participants tend to eat more in after-dinner snacks than at any other time-points during their study, and subsequently gain weight (Markwald et al., 2013; Nedeltcheva et al., 2009). It is difficult in these studies, however, to disassociate the separate impact of sleep timing and duration with the timing of caloric intake. To better understand this relationship, we tracked the timing and duration of sleep for 30 days in a group of young adults and asked that they use a photographic food diary phone application for 7 days (McHill et al., 2019; McHill et al., 2017). Importantly, the food diary time-stamped when participants ate calories, so we could identify how food timing might play a role in changes to metabolic health. Participants also visited the laboratory for an overnight stay in order for us to collect the onset of the hormone melatonin, a precise marker of an individual’s internal biological clock. Interestingly, we found a significant relationship between a higher body fat composition and the proximity of calorie consumption (consuming most of the day’s calories) relative to melatonin onset, such that the later a person ate the higher their body fat composition. However, no relationships were observed between body fat composition and the number of calories a person eats, their sleep timing, or duration. We also found that when participants slept later, they also ate later, potentially suggesting that a later sleep timing could promote later food consumption, or vice-a-versa. These findings also make sense from a food craving perspective, as our internal biological clock actually promotes hunger in the evening hours (Scheer, Morris, & Shea, 2013) and sleep restriction in the laboratory likely elongates the time a person is awake when hunger is higher (McHill, Hull, McMullan, & Klerman, 2018). Mechanistically, we think that eating later is accompanied by a reduced energetic response to the meal (i.e., Diet Induced Thermogenesis) (McHill et al., 2014), and over time this could lead to detriments in metabolic health.
Currently, we are working to further tease apart the relationships between sleep, meal timing, and cardiometabolic health and well-being by exploring how these variables all change in concert among people who are making a transition into shift work (NHLBI grant# R01 HL105495 [Olson, PI] K01 HL146992 [McHill, PI]). Shift work (working outside traditional 9am-5pm hours) inherently disturbs sleep and alters eating patterns due to the nature of working when our internal biological clocks are promoting sleep. This model of studying new shift workers is a type of natural experiment that happens in several industries, and will allow us to examine the contributions of several factors that may lead to poorer health and well-being. We are in the early stages of this project, but are optimistic that the findings will help us design smarter and more effective future interventions.
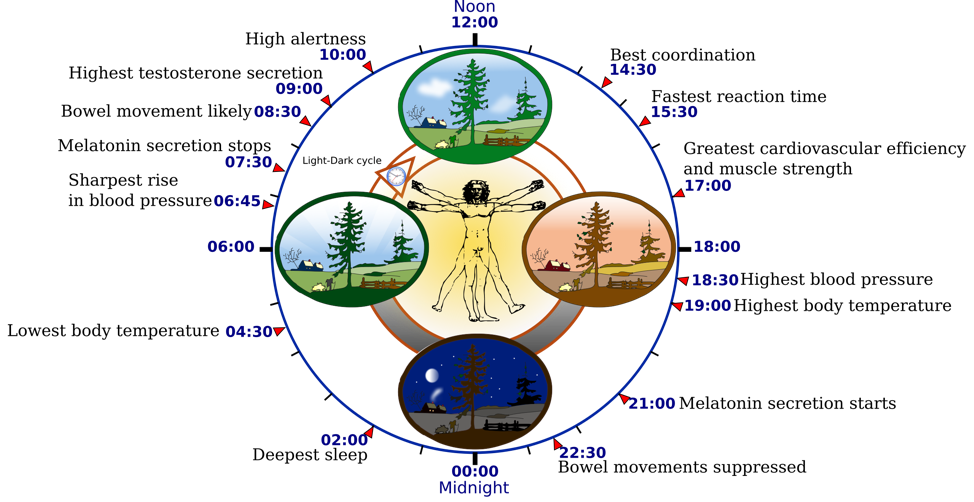
Figure. Example of how the internal biological clock can influence many aspects of physiology and behavior for someone that awakens in the morning and sleeps at night. Do note that other factors, such as light exposure, can alter these rhythms. From Wikimedia Commons, the free media repository; CC BY-SA 3.0.
Interventions to Improve Sleep and Health
For those who work part or full time, the workplace can have a profound impact on sleep duration and quality. For example, 30% of workers who report high work strain (high demands, low control) experience insomnia compared to about 5% of workers with low work strain (Kalimo, Tenkanen, Härmä, Poppius, & Heinsalmi, 2000). The impact of work arrangements on sleep has perhaps been most powerfully demonstrated by the dramatic work schedule experiment for knowledge workers caused by the global COVID-19 pandemic. Stay-at-home orders caused millions of knowledge workers to transition to 100% (or near 100%) time working from home. At the same time, schools sent children home for 100% distance or remote learning. Many schedule-driven family activities, like commuting to and from work, and transporting kids to and from school and extra-curricular events, were deleted. In a study of thousands of US residents during the first weeks of the COVID-19 pandemic, the onset of stay-at-home orders was associated with a 20-25% increase in sleep duration (Srinivasan, 2020). Some states with the biggest improvements in sleep were also those with higher average work commute times (which were no longer part of the daily routine). Moreover, recent findings with college students have found that they are sleeping ~30 minutes more on both school and free days, and with increased regularity in sleep timing (Wright et al., 2020). This suggests that many people during this global natural experiment (including workers and students) may not be setting their alarm clocks, and are sleeping until they naturally awake.
Interventions designed around allowing students and workers to align their sleep and wakefulness better with their internal biological clock, as is happening for many (but not all) people during COVID-19, have had great success. In Seattle, simply delaying school start times by ~ 1 hour, and thus allowing high school students to sleep longer, resulted in significant improvements in grades and decreases in tardiness and absences (Dunster et al., 2018). Importantly, students from lower socioeconomic status neighborhoods saw greater benefits from this simple intervention. For workers, aligning the timing of work schedules with a workers’ internal biological clock, and thus allowing for lower misalignment between work and sleep schedules, has been shown to increase sleep durations and improve well-being (Vetter, Fischer, Matera, & Roenneberg, 2015) and health (Czeisler, Moore-Ede, & Coleman, 1982).
Before the pandemic, the second author was involved in a workplace intervention for knowledge workers (Olson et al., 2015) that involved a number of factors, including supervisor training in supportive supervision, employee training and group activities, and a policy change allowing employees to work when and wherever they wanted, as long as they produced their work results (Kossek, Wipfli, Thompson, & Brockwood, 2017). Sleep was not an explicit target of the intervention, but intervention employees averaged about 8 minutes more sleep per night 12 months after baseline, and about 15 minutes more sleep per night 18 months after the intervention. The final stabilized intervention effect roughly translates into almost 2 extra hours of sleep each week. We have another current intervention trial focused on commercial team truck drivers (dyads), where one member drives while their partner sleeps in a moving semi-truck (NIOSH grant# U19 OH010154). In this project, we are evaluating a novel therapeutic mattress, which may alter disturbing vibration exposures, as well as a behavioral intervention to boost sleep quality through improved physical activity and sleep hygiene practices.
Conclusion
Sufficient sleep, and the proper timing of behaviors relative to the internal biological clock, are fundamental to the optimal functioning of almost every physiological body process. Researchers from a variety of backgrounds are needed to advance our knowledge and improve interventions in this area, including physiologists and behavioral psychologists. Together we can continue to investigate and better understand the importance of sleep and related physiological processes, as well as their interactions with our daily behaviors and associated long-term health and safety outcomes. If the goal of an intervention is to change behavior and advance health and safety, we believe there is great benefit for intervention designers to consider how sleep, and the systems and conditions that impact it, might be involved. Considering factors such as work and school schedules, stress exposures, individual sleep habits, and the timing of health behaviors and intervention activities relative to the biological clock, may all help enhance interventions and maximize their effects.
 Dr. Andrew McHill is a Research Assistant Professor within the Oregon Institute of Occupational Health Sciences at Oregon Health & Science
Dr. Andrew McHill is a Research Assistant Professor within the Oregon Institute of Occupational Health Sciences at Oregon Health & Science
University. He received his PhD at the University of Colorado Boulder and completed his post-doctoral fellowship training at Harvard Medical School and the Brigham and Women’s Hospital. His current research is interested in understanding why insufficient sleep and being awake during the night lead to poorer health and impaired cognitive performance. He has published numerous scholarly articles pertaining to how modern technology influences the human biological clock and how metabolism changes when calories are consumed at night.
- Professor, Oregon Institute of Occupational Health Sciences, Oregon Health & Science University (OHSU)
- Professor, OHSU-Portland State University (PSU), School of Public Health
- Affiliated Faculty, PSU Department of Psychology
Dr. Olson is a behavioral and occupational health psychologist whose research is focused on safety and health interventions for isolated and vulnerable working populations. He has developed unique and effective interventions for commercial drivers and home care workers, but has also conducted research with many other vulnerable and/or high-risk populations. He earned his bachelor’s degree in Psychology at Utah State University and advanced degrees in Industrial and Organizational Psychology and Applied Behavior Analysis at Western Michigan University. Dr. Olson is the current Co-Director (with Leslie Hammer) of the Oregon Healthy Workforce Center– a NIOSH Center of Excellence in Total Worker Health® (grant #U19OH010154). He is also the multiple Principal Investigator (with Curtis Cude) for Oregon’s NIOSH-funded Occupational Public Health Program (grant #U60 OH008472), where he leads the Oregon Fatality Assessment and Control Evaluation sub-project.
References
Apostolopoulos, Y., Sonmez, S., Shattell, M. M., & Belzer, M. (2010). Worksite-induced morbidities among truck drivers in the United States. AAOHN journal : official journal of the American Association of Occupational Health Nurses, 58(7), 285-296. doi:10.3928/08910162-20100625-01
Barger, L. K., Ayas, N. T., Cade, B. E., Cronin, J. W., Rosner, B., Speizer, F. E., & Czeisler, C. A. (2006). Impact of extended-duration shifts on medical errors, adverse events, and attentional failures. PLoS Medicine, 3(12), e487. doi:10.1371/journal.pmed.0030487
Barger, L. K., Cade, B. E., Ayas, N. T., Cronin, J. W., Rosner, B., Speizer, F. E., & Czeisler, C. A. (2005). Extended work shifts and the risk of motor vehicle crashes among interns. New England Journal of Medicine, 352(2), 125-134. doi:10.1056/NEJMoa041401
Czeisler, C. A., Moore-Ede, M. C., & Coleman, R. H. (1982). Rotating shift work schedules that disrupt sleep are improved by applying circadian principles. Science, 217(4558), 460-463. doi:10.1126/science.7089576
Dunster, G. P., de la Iglesia, L., Ben-Hamo, M., Nave, C., Fleischer, J. G., Panda, S., & de la Iglesia, H. O. (2018). Sleepmore in Seattle: Later school start times are associated with more sleep and better performance in high school students. Science Advances, 4(12), eaau6200-eaau6200. doi:10.1126/sciadv.aau6200
Hafner, M., Stepanek, M., Taylor, J., Troxel, W. M., & Van Stolk, C. (2017). Why sleep matters-The economic costs of insufficient sleep: A cross-country comparative analysis. Rand Health Quarterly, 6(4), 11-11. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5627640/
Kalimo, R., Tenkanen, L., Härmä, M., Poppius, E., & Heinsalmi, P. (2000). Job stress and sleep disorders: findings from the Helsinki Heart Study. Stress Medicine, 16(2), 65-75. doi:10.1002/(sici)1099-1700(200003)16:2<65::Aid-smi834>3.0.Co;2-8
Kossek, E. E., Wipfli, B., Thompson, R., & Brockwood, K. (2017). The Work, Family, and Health Network organizational intervention: Core elements and customization for diverse occupational health contexts. In F. T. Leong, D. E. Eggerth, C. H. Chang, M. A. Flynn, J. K. Ford, & R. O. Martinez (Eds.), Occupational Health Disparities: Improving the Well-being of Ethnic and Racial Minority Workers(pp. 181-215). Washington, DC, US: American Psychological Association.
Landrigan, C. P., Rothschild, J. M., Cronin, J. W., Kaushal, R., Burdick, E., Katz, J. T., . . . Czeisler, C. A. (2004). Effect of reducing interns’ work hours on serious medical errors in intensive care units.New England Journal of Medicine, 351(18), 1838-1848. doi:10.1056/NEJMoa041406
Markwald, R. R., Melanson, E. L., Smith, M. R., Higgins, J., Perreault, L., Eckel, R. H., & Wright, K. P., Jr. (2013). Impact of insufficient sleep on total daily energy expenditure, food intake, and weight gain. Proceedings of the National Academy of Sciences of the United States of America, 110(14), 5695-5700. doi:10.1073/pnas.1216951110
McHill, A. W., Czeisler, C. A., Phillips, A. J. K., Keating, L., Barger, L. K., Garaulet, M., . . . Klerman, E. B. (2019). Caloric and macronutrient intake differ with circadian phase and between lean and overweight young adults. Nutrients, 11(3), 587. doi:10.3390/nu11030587
McHill, A. W., Hull, J. T., McMullan, C. J., & Klerman, E. B. (2018). Chronic insufficient sleep has a limited impact on circadian rhythmicity of subjective hunger and awakening fasted metabolic hormones. Frontiers in Endocrinology, 9, 319-319. doi:10.3389/fendo.2018.00319
McHill, A. W., Melanson, E. L., Higgins, J., Connick, E., Moehlman, T. M., Stothard, E. R., & Wright, K. P., Jr. (2014). Impact of circadian misalignment on energy metabolism during simulated nightshift work. Proceedings of the National Academy of Sciences of the United States of America, 111(48), 17302-17307. doi:10.1073/pnas.1412021111
McHill, A. W., Phillips, A. J., Czeisler, C. A., Keating, L., Yee, K., Barger, L. K., . . . Klerman, E. B. (2017). Later circadian timing of food intake is associated with increased body fat. The American Journal of Clinical Nutrition, 106(5), 1213-1219. doi:10.3945/ajcn.117.161588
McHill, A. W., & Wright, K. P., Jr. (2017). Role of sleep and circadian disruption on energy expenditure and in metabolic predisposition to human obesity and metabolic disease. Obesity Reviews, 18 Suppl 1, 15-24. doi:10.1111/obr.12503
Nedeltcheva, A. V., Kilkus, J. M., Imperial, J., Kasza, K., Schoeller, D. A., & Penev, P. D. (2009). Sleep curtailment is accompanied by increased intake of calories from snacks. American Journal of Clinical Nutrition, 89(1), 126-133. doi:10.3945/ajcn.2008.26574
Olson, R., Crain, T. L., Bodner, T., King, R., Hammer, L. B., Klein, L., . . . Buxton, O. (2015). A workplace intervention improves actigraphic sleep duration in a randomized, controlled trial: Results from the Work, Family, and Health Network Study. Sleep Health, 1, 55-65. doi:https://doi.org/10.1016/j.sleh.2014.11.003
Olson, R., Thompson, S. V., Wipfli, B., Hanson, G., Elliot, D. L., Anger, W. K., . . . Perrin, N. A. (2016). Sleep, dietary, and exercise behavioral clusters among truck drivers with obesity: Implications for interventions. Journal of Occupational and Environmental Medicine, 58(3), 314-321. doi:10.1097/JOM.0000000000000650
Scheer, F. A. J. L., Morris, C. J., & Shea, S. A. (2013). The internal circadian clock increases hunger and appetite in the evening independent of food intake and other behaviors. Obesity (Silver Spring, Md.), 21(3), 421-423. doi:10.1002/oby.20351
Srinivasan, M. (2020, March 30). COVID pulse survey report #2. Retrieved from https://medium.com/myachievement/covid-pulse-survey-report-2-4a4121565492
Vetter, C., Fischer, D., Matera, Joana L., & Roenneberg, T. (2015). Aligning work and circadian time in shift workers improves sleep and reduces circadian disruption. Current Biology, 25(7), 907-911. doi:https://doi.org/10.1016/j.cub.2015.01.064
Wright, K. P., Linton, S. K., Withrow, D., Casiraghi, L., Lanza, S. M., de la Iglesia, H., . . . Depner, C. M. (2020). Sleep patterns during stay-at-home orders/Social distancing in response to the coronavirus COVID-19 Pandemic. Current Biology.

 Ryan Olson, PhD
Ryan Olson, PhD